
by Matt | Mar 5, 2019 | Lead in Water in Schools
This post is sponsored by Elkay.
Since Flint, Michigan, shocked the country with the severity of its lead contamination in drinking water, states and towns across the country have begun testing and remediation programs in their schools to make sure the water is safe for consumption.
What they have found is cause for concern. Lead contamination has been found in school water across the country, from New York to Arizona to California, since 2015. Though there is no national data showing how many schools or daycare centers are affected, some experts have estimated that up to 20% could contain harmful levels of lead in their water.
Schools are at high risk for lead in water due to their old infrastructure and young demographics. Lead is most likely to enter water from aging pipe infrastructure that contains lead. To make things worse, lead can cause its most severe health effects in young children, harming the way they learn, develop and behave.
Greenfield, Massachusetts, is a small, tree-lined town in western Massachusetts. The Greenfield Public School system contains a preschool and daycare center. Each day, 105 children between the ages of three and five years old attend the Academy of Early Learning.
In 2016, Greenfield officials found elevated lead levels throughout the town’s school system.
Unlike many schools that have been in the news, Greenfield quickly and transparently responded to the problem. This is the story of how they tested, strategized, and remediated the lead contamination to make water safer for all of their students, from the youngest to the oldest.
Greenfield had voluntarily tested most taps in its schools for years by measuring lead levels at two taps per school building per year. When a $2 million grant program sponsored by the Massachusetts Clean Water Trust announced that it would test public schools for free in 2016, the school system accepted the funding to conduct a more rigorous testing protocol.
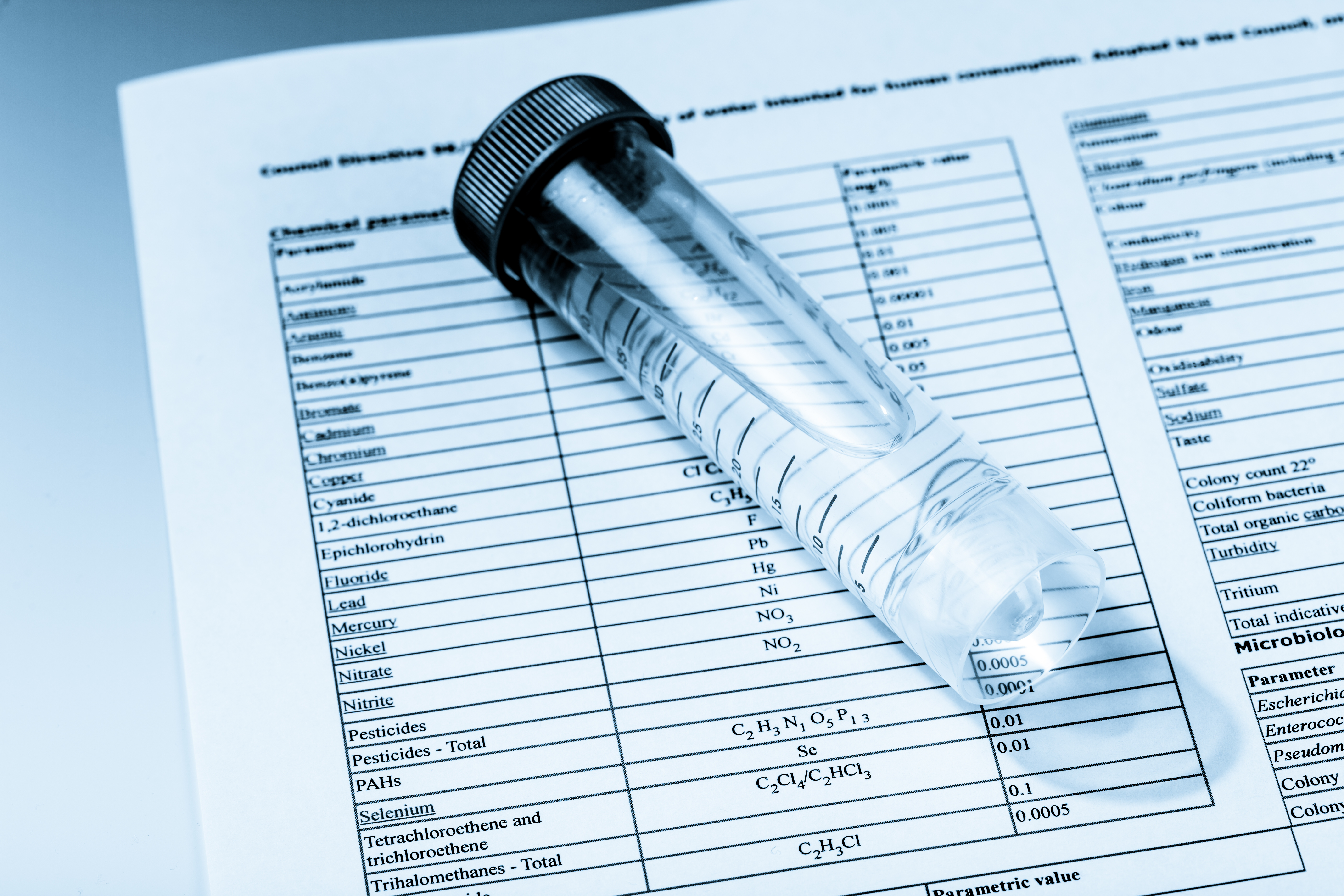
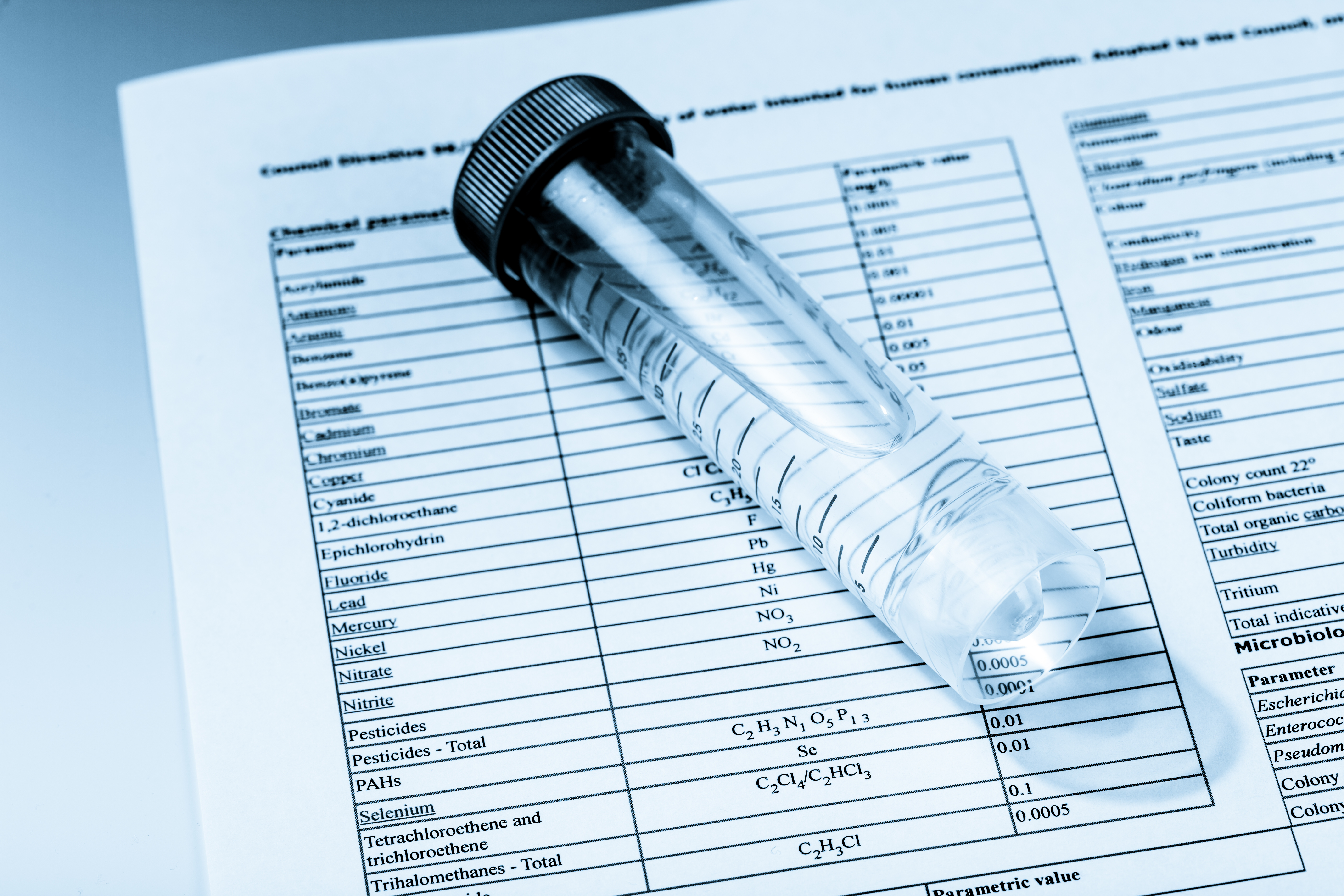
With the grant, in January 2017 school and state employees tested every fixture throughout the six school buildings for lead and copper, even rarely used taps in locations such as janitors’ rooms. In total, more than 1,000 taps were tested. Employees used a standard testing protocol by drawing samples after letting water sit in pipes for 24 hours, then drawing once more after flushing the taps.
Lab results revealed high lead levels in 25 fixtures throughout the schools. Five of these were in the Academy of Early Learning, and two were drinking fountains, endangering students as young as 3 years old.
Lead levels in faucets were found to be as high as 310 parts per billion, twenty times the EPA’s action level of 15 ppb. Drinking water sources all showed lower levels, ranging from 16 ppb to 46 ppb. In the Academy of Early Learning, the highest drinking water level found was 24 ppb.
The immediate steps to take were clear, according to Alan Schmidt, Facilities Manager at Greenfield Public Schools: “If you run into lead, the first thing you do is shut that thing down, doesn’t matter where it is.” Acting quickly, officials disconnected all of the affected fixtures within 24 hours.
Then, Greenfield methodically determined a longer-term solution. First, administrators sent a letter to parents, students, and staff notifying them of the issue and assuring them that the administration was working in a thorough and timely manner. This would be the first of three public letters to update the community, which would provide information along with social media posts, local news articles, and mentions at town meetings. Then, for the experienced Department of Public Works and facilities teams, there was a choice: which of the three main remediation options to use.
They quickly ruled out the first option, pipe replacement. This is a method (used by Newton Public Schools, for example) to remove sources of lead from pipe infrastructure. Because so few fixtures tested high for lead in Greenfield, the administration concluded that elevated levels were most likely coming from the fixtures themselves, rather than the underlying pipes. Plus, for many schools, pipe replacement is an extremely expensive and time-consuming remediation method.
The second option, which would be the least expensive up front, but also the most arguably labor-intensive and least safe, would be to flush each tap for at least 30 seconds and up to several minutes at the start of each day. This is intended to remove overnight lead buildup in pipes. Flushing is not considered a safe remediation method, however: in one 2016 study, lead concentrations at a university’s faucets returned to dangerous levels within 15-20 minutes of flushing. Greenfield did decide to implement a flushing regimen for drinking water sources testing high for copper, while waiting for hydrated lime to coat the interiors of the pipes as an anti-corrosion mechanism.
For fixtures with elevated lead levels, Greenfield officials instead chose point-of-use filtration. Greenfield used Elkay-brand drinking fountains and filtered bottle filling stations. Bottle filling stations were installed in three schools, including the Academy of Early Learning. According to Ouellette, the choice was clear based on efficacy and cost.
These units contain filters that are NSF certified to remove over 99% of lead. They require a simple filter replacement one year after installation or possibly more depending on water usage.
The new bottle filling stations were also a solution within the means of the town budget. According to Ouellette, in total the remediation cost approximately $12,000 between testing, replacement of about 20 fountains, and removal of about six drinking fountains that were old and infrequently used. Town engineers and plumbers donated their time to install the replacement fixtures free of charge.
At sinks and other sources of non-potable water, officials posted signage to warn students and staff away from drinking from them.
By September 2017, with new filtered bottle filling stations installed, a new round of testing confirmed that Greenfield’s water was within the level of consumption considered safe to drink, every fixture testing at a lead concentration of 6ppb or below. The town breathed a sigh of relief. According to Jordana Harper, Superintendent of Greenfield Public Schools, the community and school administrators were pleased with the swiftness and comprehensiveness of the response. “Knowledge is power,” she says, “and ensuring the safety of our schools is a top priority.”
The newly installed fixtures have passed two rounds of testing since September 2017. Using their new knowledge and protocols, the school district will continue to make sure water remains cleaner and safer.
Testing it is the only way to find out if there are harmful amounts of lead in your water.
Greenfield Public Schools’ lead remediation strategy is just one way to respond to a systemic problem, but studying their methods provides valuable lessons on how to handle the problem of lead in drinking water in schools.
1. Test thoroughly and beyond what is legally required
Federal regulations do not require any specific lead testing for 90% of schools in the U.S. Even though the town DPW had regularly tested taps throughout Greenfield Public Schools, some fixtures emitting lead-contaminated water were not identified until the Massachusetts Clean Water Trust grant in 2016. Sometimes the most rarely used fixtures are the least obvious choices for lead testing, but can discharge the most dangerous lead levels, since lead may be allowed to collect in pipes for long periods of time. Luckily, this testing program provided enough funding to collect samples from every fixture, including rarely used fixtures, so that the schools could address the issue.
2. Know the options
Greenfield schools were able to quickly analyze their priorities – cost-effectiveness, efficacy and ADA-compliance. They chose a solution that best addressed these, Elkay fountains and filtered bottle fillings stations, because school officials were familiar with the three main options for lead remediation.
For more information about the options for remediating lead contamination of school drinking water, please read “How to Solve Your School’s Lead in Water Problem.”
3. Build systems for long-term safety
The process of responding to lead contamination made it clear that Greenfield’s previous testing system had been valuable, but incomplete, as it had missed some lead contamination by only testing two fixtures in each building per year and prioritizing the most commonly used fixtures. Now, with the baseline provided by the Massachusetts statewide testing program, officials will continue to use this system moving forward but will be prepared to expand testing if it becomes necessary. It will be important to maintain clear records of the testing so that the information may be easily referenced.
With its swift and decisive response, Greenfield Public School officials succeeded in making water safer for all students, from the youngest to the oldest.
In addition to Greenfield Public Schools, BeCause Water has learned from schools across the country and assisted with testing, fundraising, remediation and awareness. For additional resources and information, please contact us at support@becausewater.org
NPR, April 2016. “Lead-Laced Water In Flint: A Step-By-Step Look At The Makings Of A Crisis.”
US EPA, National Service Center for Environmental Publications, 1989. “Lead Ban: Preventing the Use of Lead in Public Water Systems and Plumbing Used for Drinking Water.”
US EPA. “Basic Information About Lead in Drinking Water.”
USA TODAY, March 2016. “Got lead in your water? It’s not easy to find out.”
Water Research Center. “Special Report #3: Lead In Drinking Water – Is There Lead In My Drinking Water?”
Mayo Clinic. “Lead Poisoning Symptoms and Causes.”
Pediatrics Journal, October 2005. “Lead Exposure in Children: Prevention, Detection, and Management.”
Agency for Toxic Substances and Disease Registry, August 2007. “PUBLIC HEALTH STATEMENT: Lead.”
US EPA. “Drinking Water Requirements for States and Public Water Systems: Lead and Copper Rule.”
US EPA. “Consumer Confidence Reports (CCR).”
US Government Publishing Office, June 1991. “Title 40: Protection of Environment; Part 141: National Primary Drinking Water Regulations; Subpart 1: Control of Lead and Copper.”
USA TODAY, March 2016. “Beyond Flint: Excessive lead levels found in almost 2,000 water systems across all 50 states.”
Massachusetts Water Resources Authority. “What You Need to Know About Lead In Tap Water.”
CNN, June 2016. “5,300 U.S. water systems are iUS authorities distorting tests to downplay lead content of watern violation of lead rules.”
Natural Resources Defense Council, June 2016. “Report: What’s in Your Water? Flint and Beyond Analysis of EPA Data Reveals Widespread Lead Crisis Potentially Affecting Millions of Americans.”
The Guardian, January 2016. “US authorities distorting tests to downplay lead content of water.”
US EPA Office of Enforcement and Compliance Assurance, December 2009. “Memorandum: Drinking Water Enforcement Response Policy.”
CNN, March 2016. “Flint water crisis lawsuits: 5 things to know.”

by Matt | Mar 5, 2019 | Lead in Water in Schools
This post is sponsored by Elkay.
After Flint, Michigan, shocked the country in 2015 with the severity of lead contamination in its drinking water supply, states and towns across the country have implemented testing and remediation programs in their schools to make sure the water is safe.
The lead problem is even more widespread than anyone anticipated, reaching not only K-12 public school systems, as in Flint, but colleges and universities as well.
Rowan University is a public university spread across three suburban campuses in Glassboro, Camden, and Stratford, New Jersey. Approximately 14,000 undergraduate students live and study there. When lead was identified in one classroom building on the Glassboro campus in 2016, the university spent more than a year deftly testing and remediating the problem. The university committed to complete transparency throughout the process.
Colleges and universities face different challenges and opportunities than local public school districts. This is their story.
Lead in Water at Colleges and Universities:
Lead is a neurotoxin that damages the health of young adults. The risks of lead exposure are generally most severe for young children, and news of lead contamination in children’s school drinking water is a heartbreaking public health problem. The United States’ National Institutes of Health recognizes lead as a “serious threat” to adults as well, as it accumulates slowly in our bodies and damages our neurological, gastrointestinal and reproductive systems.
There are no federal laws requiring higher education institutions to test for lead in drinking water. New Jersey does not require this testing either, so Rowan University had tested its on-campus daycare center for lead in drinking water annually, but had never sampled for lead in water in any other buildings. Lead in water usually comes from corrosion of water mains and plumbing within buildings, and contamination outside of the daycare center went unnoticed.
In July 2016, the Facilities Department received complaints of discolored water at Linden Hall. Curious, the team tested taps throughout the building for contaminants. The samples identified iron as the cause for discoloration. At the same time, they detected the presence of lead. University administrators knew that they needed to keep testing.
Testing proceeded in nearby buildings. As soon as those results came back in August 2016, the university contacted the New Jersey Department of Environmental Protection. Rowan University had a lead problem.
With the help of the NJDEP, administrators notified the community and began to develop a plan to test the rest of campus.
The university moved quickly. It hired Pennoni, a certified consulting company, to assist with the testing plan. In the meantime, the staff took “grab” samples to simply detect the presence of lead without a certified lab test process. This gave an approximate idea of the scope of the problem.
Next, the real testing began, and it continued from November 2016 through September 2017. Contractors surveyed the plumbing of each building and tested every single potable water source, following standard protocols. They analyzed more than 4,100 samples in total. They also tested some non-potable sources in order to map possible pathways of lead contamination throughout plumbing systems. The thorough approach provided safety and transparency.
Out of 43 buildings on campus, nine had test results showing lead above action levels. These elevated levels ranged from just above 15 parts per billion to more than 2,000 ppb, exceeding 130 times the EPA action level. One sink in Willow Hall, a residential building, even tested at 10,100 ppb – an extremely hazardous level higher than was found in many Flint homes.
The tests were thorough enough to reveal three main sources of contamination: fixtures, brass backflow preventers and water mains.

The administration committed to complete transparency even as the situation expanded. Joe Cardona, Vice President for University Relations, describes the initial response: “We had a phone bank set up that first night, an email line and a phone line. We handled it like it was an extreme crisis.”
Every affected fixture was disconnected from the water supply, and staff distributed bottled water to students. Between November 2016 and September 2017, roughly 400,000 bottles of water were distributed.
Rowan University assessed priorities for the response. The university’s most pressing concern was to find an effective solution. Officials focused on not only removing current sources of lead, but also any possible chances for future lead contamination. Cost played a role as well; the university only had $2 million available, and not enough money or time to replace each building’s entire pipe system.
Rowan’s remediation strategy included plumbing replacement and filtration. Within central plumbing systems, workers systematically removed water mains and backflow preventers and installed filters where appropriate. They also installed in-line ANSI/NSF-approved filters at point-of-use for all cold water sources in kitchens and sinks, even fixtures that did not have test results above EPA action levels, including 1,421 filters in residence halls alone.
Next, workers replaced the 96 affected drinking fountains with Elkay filtered bottle filling stations. Workers also fitted eight traditional drinking fountains with in-line filters. The bottle filling station filters are NSF certified to remove over 99% of lead. University staff also liked that the stations have LED light indicators that tell users whether the filter is still effective or needs to be changed (e.g., green, yellow and red lights), plus a counter that indicates how many 20 oz. plastic water bottles were saved from the trash by using the station.
The entire response to the contamination, from start to finish, cost $1.2 million dollars. By the end, every fixture tested below 15 ppb, and most fixtures registered undetectable levels. The full testing results before and after the university’s response can be found here.
Testing it is the only way to find out if there are harmful amounts of lead in your water.
The Public Relations Challenge:
Transparency might not seem like an intuitive strategy, since there has been much bad press surrounding lead contamination in the past two years. Plus, Rowan University first discovered positive lead samples only weeks before the start of the school year in 2016 – not the happiest news for new incoming students and their parents.
However, for Rowan University, transparency was a guiding principle for the process early on, as led by University President Ali Houshmand. According to Cardona, transparency has been Houshmand’s signature throughout his tenure at the university. He believes that it cultivates trust among students and the community and keeps the university accountable. During a crisis, it was even more important to keep that trust, be truthful about what was going on, and calm people’s anxieties.
Throughout the testing and remediation process, Rowan University maintained a water quality hotline, held public meetings with doctors and water quality experts, published test results online, and posted regular progress updates on the university website.
Some students were so nervous about the contamination that they refused to shower. While that was an issue, the educational resources that the colleges provided were able to clear up misinformation and ensure safety.
By the end of the remediation process in September 2017, Cardona says that transparency turned out to be a positive public relations strategy for the university, as it showcased the lengths that the university went to in order to protect students.
It also brought the university population closer together. Cardona describes the effect as: “Challenges pull organizations together. When times get rough, everybody pulls in the same direction.”
1. Test thoroughly and beyond what is legally required:
Neither federal nor New Jersey state regulations require colleges and universities to test for lead contamination in water. In May 2016, New Jersey Governor Chris Christie passed a requirement for 3,000 public schools across the state to begin testing their water for lead by fall 2016, made funding available to reimburse schools, and strengthened guidelines on school responses to children’s lead exposure. The rule went into effect at the same time as Rowan University discovered lead contamination in Linden Hall. However, this legislation does not include colleges or universities. Rowan University’s thorough testing after the first discoveries of lead contamination was critical to identifying and fully responding to the problem. Some fixtures showed much higher results than the fixtures right next to them, and the university could have missed poisonous outlets by only testing some of them. In addition, understanding lead levels near water mains and accessories like the backflow preventers helped the university understand where lead came from, and respond effectively.
2. Know the options:
Rowan University utilized two viable options for lead contamination: testing and replacing contaminated backflow preventers and water mains, and installing central and Elkay-brand point-of-use filtration. Identifying priorities was a key step for university responders. The goal of 100 percent effectiveness reassured parents, students and prospective students. Additionally, a $2 million emergency response budget allowed the university responders to sift through the options and act accordingly. For more information about the options for remediating lead contamination of school drinking water, please read : “How to Solve Your School’s Lead in Water Problem.”
3. Be transparent and include community early in the process:
By making information available while following response best practices, the university increased community feelings of safety and trust throughout the response. By maintaining online records of test results, recent updates and frequently asked questions, the university saved time from fielding questions – which was a good idea given the thousands of students, employees, parents, prospective students, journalists, and even other universities who were curious about the university’s water safety and response methodology. Other colleges and universities that are worried about lead contamination news potentially damaging admissions data or publicity can reference this case. Cardona even felt that the university’s public image was better than before, though admissions data has yet to be released for the years following the initial lead discovery. Following these guidelines, Rowan University successfully returned safer water to its students. BeCause Water has learned from schools across the country and assisted with testing, fundraising, remediation, and awareness. For additional resources and information, please contact us at : support@becausewater.org.
NPR, April 2016. “Lead-Laced Water In Flint: A Step-By-Step Look At The Makings Of A Crisis.”
US EPA, National Service Center for Environmental Publications, 1989. “Lead Ban: Preventing the Use of Lead in Public Water Systems and Plumbing Used for Drinking Water.”
US EPA. “Basic Information About Lead in Drinking Water.”
USA TODAY, March 2016. “Got lead in your water? It’s not easy to find out.”
Water Research Center. “Special Report #3: Lead In Drinking Water – Is There Lead In My Drinking Water?”
Mayo Clinic. “Lead Poisoning Symptoms and Causes.”
Pediatrics Journal, October 2005. “Lead Exposure in Children: Prevention, Detection, and Management.”
Agency for Toxic Substances and Disease Registry, August 2007. “PUBLIC HEALTH STATEMENT: Lead.”
US EPA. “Drinking Water Requirements for States and Public Water Systems: Lead and Copper Rule.”
US EPA. “Consumer Confidence Reports (CCR).”
US Government Publishing Office, June 1991. “Title 40: Protection of Environment; Part 141: National Primary Drinking Water Regulations; Subpart 1: Control of Lead and Copper.”
USA TODAY, March 2016. “Beyond Flint: Excessive lead levels found in almost 2,000 water systems across all 50 states.”
Massachusetts Water Resources Authority. “What You Need to Know About Lead In Tap Water.”
CNN, June 2016. “5,300 U.S. water systems are US authorities distorting tests to downplay lead content of wate violation of lead rules.”
Natural Resources Defense Council, June 2016. “Report: What’s in Your Water? Flint and Beyond Analysis of EPA Data Reveals Widespread Lead Crisis Potentially Affecting Millions of Americans.”
The Guardian, January 2016. “US authorities distorting tests to downplay lead content of water.”
US EPA Office of Enforcement and Compliance Assurance, December 2009. “Memorandum: Drinking Water Enforcement Response Policy.”
CNN, March 2016. “Flint water crisis lawsuits: 5 things to know.”

by Matt | Mar 5, 2019 | Lead in Water in Schools
Whether you’re a school administrator, teacher or concerned parent, the topic of lead in drinking water can be very concerning, overwhelming and complex. As a 501(c)(3) nonprofit whose mission is to help communities improve access to clean drinking water, we have fielded many questions regarding this topic. Here are answers to the most popular questions.
Q: Are schools required to test for lead in water?
A: The majority of states do not require schools to test their drinking water for lead. This, along with insufficient funding and education for water infrastructure, arguably explains why we feel there is a lead crisis in U.S. schools. If it weren’t for the media attention surrounding lead levels in water in Flint, Michigan, there could still be very little awareness about the issue.
Fortunately, there is progress is being made as states and municipalities are beginning to establish their own regulations for testing drinking water for lead. Illinois, New Jersey, and New York are some of the first states to implement these new policies.
Q: How bad is the lead in water situation in schools?
A: The U.S. Government Accountability Office conducted a country-wide poll for lead in schools’ drinking water in 2017. They found that 43% of districts, serving 35 million students, tested for lead. Of those, 37% discovered elevated lead levels and reduced or eliminated exposure.
Combining the probability of finding lead in school’s drinking water with the fact that children are at the highest health risk for lead poisoning, is cause for major concern.
Q: Is flushing a safe method to remediate lead in drinking water?
A: Although some schools might use flushing as a way to address their lead problem, the effectiveness of this method is questionable. New research out of Polytechnique Montreal in Quebec, Canada shows that unsafe lead levels may return within 30 minutes after flushing.
Q: What level of lead in drinking water is considered safe?
A: The Environmental Protection Agency (EPA) sets the action level for lead in drinking water at 15 parts per billion (ppb). However, their minimum contamination level goal (MCLG) is set at zero.
The World Health Organization’s (WHO) guideline is 10 parts per billion (ppb).
The American Academy of Pediatrics (AAP) recommends schools set their limits at 1 part per billion (ppb). The states of Washington and Massachusetts both have pending legislation that could implement protective policies to assure lead levels adhere to the 1 part per billion (ppb) maximum contamination level. Both Washington D.C. and San Diego have a policy of 5 parts per billion (ppb) for their school’s water.
Q: What is the best way to address the issue of lead in drinking water in schools?
A: There are two methods that we would recommend schools to consider when it comes to lead remediation.
The first option to consider is remediation through removing the source of lead, which may include the removal of lead by replacing service lines, internal piping, or lead-bound fixtures. While this solution is very effective, it can be extremely expensive and take one year or more to complete.
The second option to consider is point-of-use filtration. Elkay®, a trusted name in water delivery for more than four decades, offers point- of-use bottle filling stations with filters that are NSF certified to NSF/ANSI 42 and 53 for reduction of lead, Class 1 particulate, chlorine, taste and odor.
Q: What are the health dangers of being exposed to lead in drinking water?
A: Lead is harmful to health, especially in children, and can result in lowered IQ, behavioral problems, brain damage and more.
Q: As a school, how can I test my drinking water for lead?
A: The best way to test your school’s drinking water for lead is to work with a state-certified lab. The EPA’s website provides a list of certified labs by state. Many states or cities have free testing programs so check with your local agencies.
If you have additional questions about lead in drinking water, please leave a comment below and we’ll do our best to respond with an answer as soon as possible.

by Matt | Jul 11, 2018 | Lead in water
Recently, there has been an uptick in the number of schools discovering elevated lead levels in their drinking water. In response, many are learning that filtered bottle filling stations can be an effective, efficient, and affordable way to restore safe drinking water to their students and staff.
Given that bottle fillers are a relatively new technology, the purpose of this guide is to answer common questions and outline the simple steps for proper system maintenance.
Read the full guide HERE.
by Matt | Apr 20, 2015 | Local Water Protection, water and health
by: Amanda Sebert
When astronomers search for life on another planet, what they are really looking for is water. Water is essential to all life, and unless it is clean, we cannot consider it water. As a species, we have learned from our evolutionary history, and from recent tragedies like the Ebola outbreak in West Africa,
 that polluted water sources can cause significant harm to both human health and the environment. Keeping dangerous chemicals out of our water sources is an obvious goal, but in the toxin-filled world in which we live, it can be harder than you might think.
that polluted water sources can cause significant harm to both human health and the environment. Keeping dangerous chemicals out of our water sources is an obvious goal, but in the toxin-filled world in which we live, it can be harder than you might think.
Everything we put on and in our bodies will ultimately end up in our waterways. It can be difficult to see the connection between products we use on our bodies and their affects on our environments. The lotion that helps brighten your skin may contain parabens that are disrupting your hormones. Extensive scientific studies have shown that hormone systems of wildlife are disrupted by chemicals from personal care products that end up in water bodies after being rinsed down the drain. These same water sources may be the drinking water supply for hundreds or thousands of people. One need not be a scientist to understand the connection between our health and our water sources.
Personal care products are those used for hygiene and beautification. We use personal care products such as, toothpaste, hand soap, mascara, and deodorant. Everyone who uses these products are exposed to dangerous toxins like parabens, phthalates, formaldehyde, triclosan, tocopheryl acetate, and many more. The Campaign for Safe Cosmetics has found that the average American uses 9 personal care products daily. In these 9 products, there are approximately 126 unique chemical ingredients. Scientific research is lacking when it comes to understanding how the chemicals in these products interact with each other or with the other toxins we are exposed to in our daily lives.

The Environmental Working Group, an organization made up of scientists, policy experts, lawyers, communication experts and programmers, has found that more than one-third of all personal care products contain at least one ingredient linked to cancer. Unfortunately, cancer is not the only health problem; toxins in personal care products have been linked to many different health issues which include birth defects and reproductive issues, respiratory conditions like asthma, behavioral disorders, hormone disruption, nervous system problems, and mental health issues such as depression. Sometimes a clear link exists between a health issue and a toxin, but that is not normally the case. For example, formaldehyde and formaldehyde-releasing preservatives are used in many personal care products, particularly in shampoos and liquid baby soaps. The formaldehyde and preservatives are used to prevent bacteria growth in these products, and these chemicals can be absorbed through the skin. Some evidence suggests that these absorbed chemicals may lead to allergic skin reactions and cancer. (Campaign for Safe Cosmetics).
Toxins in personal care products that cause adverse health impacts end up in our waterways. Thanks to modern science, public drinking water sources have the capability of removing most of these toxins before they reach consumers. This does not help the wildlife who come into contact with polluted water before it is treated. Individuals and communities who have private wells are especially at risk from toxins in water. These communities that rely on private well water may not have sophisticated water treatment systems to filter out these potential toxins.
So how can we protect ourselves from harm and also keep toxins from personal care products out of our waterways? The European Union has banned over 1,132 chemicals from personal care products of which the US has only banned 11. There is no reason for certain harmful toxins to remain in our products if safer alternatives exist and are readily available. Getting big businesses to change their ways can be a difficult and daunting task. We must use our strength in numbers to induce change by choosing personal care products that are safe for bodies and will not pollute our waterways. Visit the Skin Deep Database to see if your products are safe. Check out the Action Alerts from the Campaign for Safe Cosmetics where you can tell cosmetics companies and elected officials that safe cosmetics are important to you. We must press for legislation that: (1) requires product manufacturers to use safer alternatives (2) imposes broad regulations that protect human health and the environment and (3) keeps dangerous toxins out of our waterways.






 that polluted water sources can cause significant harm to both human health and the environment. Keeping dangerous chemicals out of our water sources is an obvious goal, but in the toxin-filled world in which we live, it can be harder than you might think.
that polluted water sources can cause significant harm to both human health and the environment. Keeping dangerous chemicals out of our water sources is an obvious goal, but in the toxin-filled world in which we live, it can be harder than you might think.
